Transverse Myelitis
What is Transverse Myelitis?
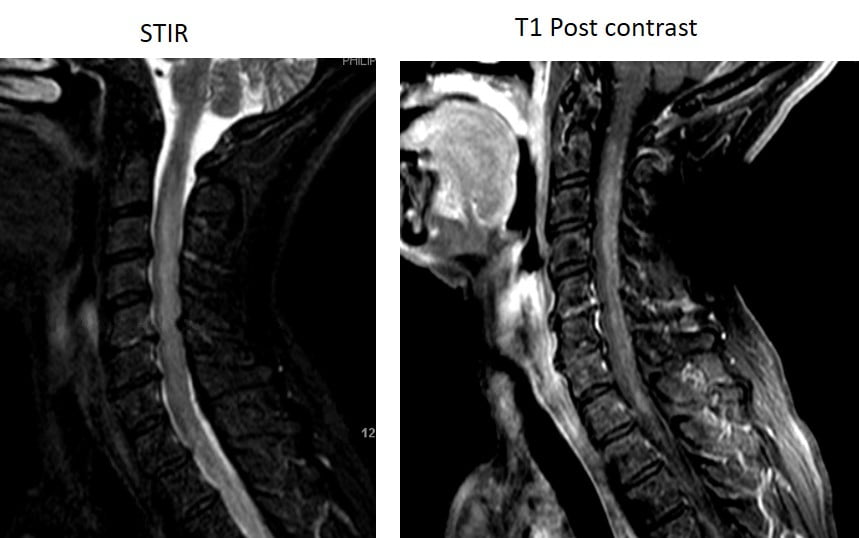
Transverse myelitis (TM) includes a large group of disorders that leads to inflammation causing injury to the spinal cord with varying degrees of weakness, sensory alterations, and autonomic dysfunction. Autonomic dysfunction affects the part of the nervous system that controls involuntary activity, such as the heart, breathing, the digestive system, and reflexes. Wide ranges of causes include infections (often viral infections), post-infectious process (inflammation triggered by the infection and not direct infection of the spinal cord by the virus), demyelinating disease (such as MS, NMOSD, MOGAD – see above), autoimmune or paraneoplastic myelitis (caused by a particular autoantibody), or other systemic inflammatory disease (such as rheumatological disease or sarcoidosis). Diagnostic work up includes imaging of the spinal cord with MRI, blood work, and a lumbar puncture to evaluate for inflammation, virus, and/or antibodies in the cerebrospinal fluid (CSF).
What are the treatment options?
Treatment depends of the cause of the transverse myelitis and can range from antiviral therapy (if due to an infectious process) to immune therapy (if due to an inflammatory process).